Introduction to Radiation Therapy
Radiation therapy is a powerful tool in the fight against cancer, using high-energy radiation to shrink tumours and kill cancer cells. While effective, it can also cause side effects that impact a patient’s quality of life. We’ll explore the common side effects of radiation therapy, the critical role cancer doctor in Nagpur plays in managing this treatment, and discuss recent advancements in the field.
Common Side Effects of Radiation Therapy
Radiation therapy affects both cancer cells and healthy cells in the targeted area. As a result, patients may experience various side effects, which can be broadly categorized as follows:
- Fatigue:
- One of the most common side effects, affecting up to 80% of patients.
- Often described as feeling physically, emotionally, and mentally exhausted.
- Usually, it begins a few weeks into treatment and may persist for weeks or months after treatment ends.
- Skin Changes:
- The treated area may become red, dry, or itchy, similar to a sunburn.
- In severe cases, the skin may blister, peel, or develop a rash.
- Usually begins within a few weeks of starting treatment and often heals within 4-6 weeks after treatment ends.
- Hair Loss:
- Hair loss occurs in the treatment area, which may be temporary or permanent.
- The extent of hair loss depends on the radiation dose and the size of the treated area.
- Hair typically starts growing back 3-6 months after treatment ends, though it may have a different texture or colour.
- Nausea and Vomiting:
- More common when radiation is directed at the abdomen or brain.
- Can be managed with antiemetic medications and dietary changes.
- Usually subsides within a few weeks after treatment ends.
- Diarrhoea:
- Often occurs when the pelvic or abdominal area is treated.
- Can lead to dehydration and nutrient deficiencies if not managed properly.
- Usually improves within a few weeks after treatment, but some patients may experience long-term changes in bowel habits.
- Mouth and Throat Problems:
- Dry mouth, difficulty swallowing, or changes in taste can occur with head and neck radiation.
- Can lead to dental problems and impact nutrition.
- Management may include special oral care routines and dietary modifications.
- Lymphedema:
- Swelling in arms or legs due to damage to the lymph nodes.
- Can occur months or years after radiation therapy.
- Managed through physical therapy, compression garments, and lifestyle modifications.
- Cognitive Changes:
- Sometimes called “chemo brain,” this can include memory problems and difficulty concentrating.
- May be temporary or long-lasting.
- Management strategies include cognitive rehabilitation and lifestyle adjustments.
- Sexual and Reproductive Issues:
- This can include decreased libido, erectile dysfunction in men, and vaginal dryness in women.
- May impact fertility, especially if radiation is directed at reproductive organs.
- Oncologists can discuss fertility preservation options before treatment begins.
- Secondary Cancers:
- A rare but serious long-term risk of radiation therapy.
- Usually occurs years after the initial treatment.
- Regular follow-ups and screenings are crucial for early detection.
It’s important to note that the severity and type of side effects can vary greatly depending on the treatment location, dosage, and individual patient factors.
The Crucial Role of Oncologists in Radiation Therapy
Oncologists specializing in radiation therapy, known as radiation oncologists, play a pivotal role throughout the treatment process:
- Treatment Planning:
- Determine the appropriate type and dose of radiation
- Use advanced imaging techniques like CT, MRI, or PET scans to map the treatment area precisely
- Collaborate with other specialists to develop a comprehensive care plan
- Utilize sophisticated treatment planning software to optimize radiation delivery
- Patient Education:
- Explain the treatment process and potential side effects in detail
- Guide managing side effects and maintaining overall health
- Discuss the expected timeline of treatment and recovery
- Address patient concerns and answer questions to ensure informed consent
- Monitoring and Adjusting Treatment:
- Regularly assess the patient’s response to therapy through imaging and physical examinations
- Make necessary adjustments to minimize side effects while maximizing treatment efficacy
- Coordinate with medical physicists to ensure precise radiation delivery
- Managing Side Effects:
- Prescribe medications to alleviate symptoms (e.g., anti-nausea drugs, pain relievers)
- Recommend lifestyle changes or supportive therapies (e.g., nutrition counselling, physical therapy)
- Coordinate with other healthcare providers for comprehensive care
- Implement strategies to protect healthy tissue during treatment
- Follow-up Care:
- Monitor for long-term side effects through regular check-ups
- Conduct regular imaging and blood tests to assess cancer recurrence risk
- Develop long-term survivorship plans
- Coordinate with primary care physicians for ongoing care
- Emotional Support:
- Provide counselling and resources to help patients cope with the psychological impact of treatment
- Refer patients to support groups or mental health professionals when needed
- Address concerns about body image changes and quality of life issues
- Research and Innovation:
- Stay updated on the latest advancements in radiation therapy
- Participate in clinical trials to improve treatment outcomes
- Contribute to the development of new radiation techniques and technologies
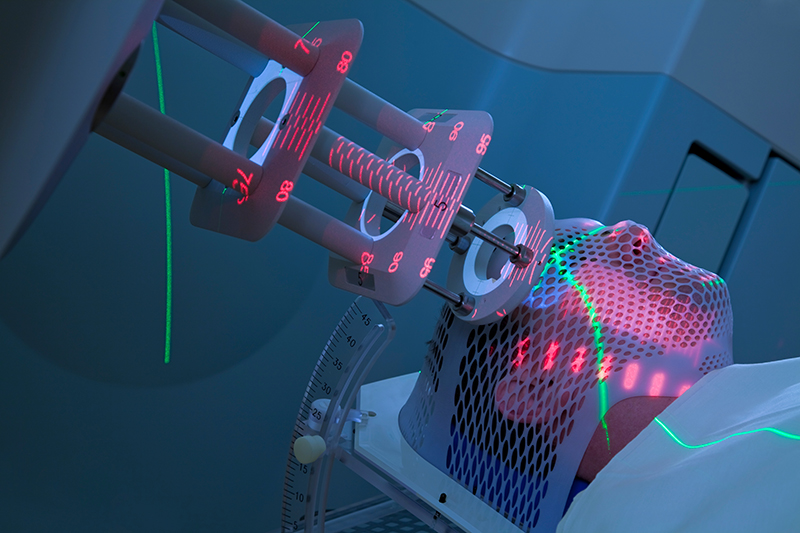
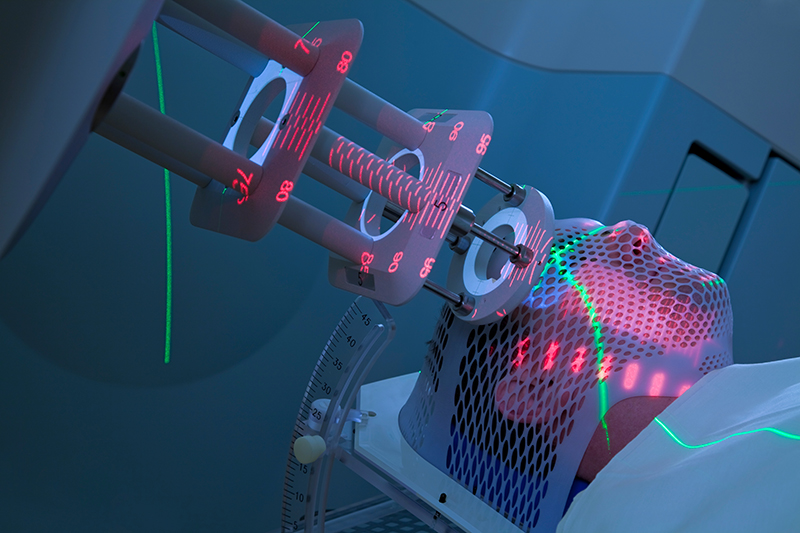
Recent Advancements in Radiation Therapy
The field of radiation oncology is rapidly evolving, with new technologies and techniques improving treatment precision and reducing side effects:
- Intensity-Modulated Radiation Therapy (IMRT):
- Allows for more precise shaping of radiation beams to conform to the tumour shape
- Reduces radiation exposure to healthy tissue, minimizing side effects
- Image-Guided Radiation Therapy (IGRT):
- Uses real-time imaging to guide radiation delivery
- Improves accuracy and allows for adjustment based on tumor movement
- Proton Therapy:
- Uses protons instead of photons to deliver radiation
- Offers better dose distribution and potentially fewer side effects
- Stereotactic Body Radiation Therapy (SBRT):
- Delivers high doses of radiation to small, well-defined tumours
- Reduces treatment duration and may improve outcomes for certain cancers
- Adaptive Radiation Therapy:
- Adjusts the treatment plan based on changes in tumour size or patient anatomy during treatment
- Improves treatment precision and may reduce side effects
Oncologists play a crucial role in implementing these advanced technologies and determining which patients are most likely to benefit from them.
Conclusion
While radiation therapy can cause challenging side effects, it remains a crucial tool in cancer treatment. The expertise of radiation oncologists is essential in maximizing the benefits of this therapy while minimizing its impact on patients’ quality of life. By working closely with their oncology team and leveraging the latest advancements in the field, patients can navigate the complexities of radiation therapy and focus on their journey towards recovery. As research continues and technology evolves, we can expect even more precise and personalized radiation treatments in the future, further improving outcomes for cancer patients.